What is a Prolapsed Disc?
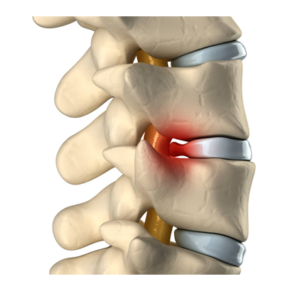
A prolapsed disc is a condition that is commonly referred to in several different ways, including a ruptured disc, a herniated disc, and a slipped disc. All of these terms are used interchangeably to indicate that a portion of a disc’s gel-like nuclear material has leaked out into the spinal canal through a tear or split in the disc’s layered, cartilaginous outer wall. This condition can occur at any level of the spine, but it is most frequently found in the lower back, where the lumbar vertebrae and discs bear much of the body’s weight, and where the body’s ongoing movements produce significant stress on the spine over time.
Disc degeneration often occurs in several stages, and disc prolapse takes place at a relatively early stage. When a disc becomes thinner, drier or weaker due to age or injury, it can begin to protrude beyond its normal position between the vertebrae. This condition can eventually lead to a full herniation, or tearing, of the disc’s outer wall and the subsequent extrusion of nuclear material.
Causes of a Prolapsed Disc
A traumatic spine injury can cause a prolapsed disc, but the condition is most often related to the normal wear and tear that occurs over time on the parts of the spine. While cumulative stress on the spine is inevitable, certain factors have been shown to increase the likelihood that an individual will develop a prolapsed disc, such as heredity, repetitive activity, prolonged inactivity, unhealthy weight, and smoking.
As part of the natural aging process, the water content within the discs slowly begins to diminish. When a disc becomes dehydrated, it loses flexibility and becomes brittle, and is less able to withstand the normal pressures being exerted by the vertebrae situated immediately above and below it. As a result, a chain reaction can occur in which the gel-like inner material (nucleus pulposus) of the compromised disc exerts pressure on the tough, fibrous outer wall (annulus fibrosus) that normally contains it. As pressure builds on the already weakened disc wall, its integrity can be compromised. A tear can begin to form — typically starting on the inside of the disc and working its way outward — and the inner-disc material can begin to force its way out through the opening, leading to a prolapsed disc.
Symptoms of a Prolapsed Disc
In many cases, a prolapsed disc is asymptomatic and remains undetected, allowing you to go about your daily life as usual. However, if the extruded disc material irritates nerve endings in the disc’s wall or impinges an adjacent nerve root or the spinal cord itself, it can produce uncomfortable symptoms like localized discomfort and radiating pain, tingling, numbness, stiffness and muscle weakness.
The symptoms that arise when extruded disc material irritates or compresses sensitive neural tissue can manifest either locally or elsewhere in the body, depending on the area of the body affected by the compressed nerve root. There are 31 pairs of nerve roots situated along the spine — which spans from the neck to the coccyx (tailbone) — including eight in the cervical region, 12 in the thoracic region, five in the lumbar region, five in the sacrum and one in the coccyx.
A prolapsed disc in the cervical region
The nerve roots in the cervical spine send signals to the head, diaphragm, upper body, arms, wrist, and hands. Therefore, a prolapsed disc in the cervical region can produce migraine headaches and other symptoms that affect the:
- Neck
- Shoulders
- Upper back
- Deltoids
- Triceps
- Biceps
- Forearms
- Wrists
- Hands
- Fingers
Thoratic Prolapsed Disc
The nerve roots in the thoracic spine send signals to the upper back, chest, torso and ribs. Because the thoracic vertebrae are relatively rigid, the discs in between those vertebrae are less susceptible to prolapse than those discs cushioning the more flexible vertebrae located in the cervical and lumbar regions. Nevertheless, when a thoracic disc prolapse occurs, it can produce symptoms that are very similar to the signs of other serious conditions, such as those affecting the heart, lungs, kidneys and gastrointestinal system. Therefore, a prompt and accurate diagnosis of the root cause of any form of chest pain, balance loss or abdominal discomfort is imperative.
Lumbar Prolapsed Disc
The nerve roots in the lumbar spine travel to the lower back, hips, buttocks, legs, ankles, feet and toes. The highly flexible vertebrae in the lower back make the discs between them especially vulnerable to degeneration and disc prolapse. A prolapsed disc in the lumbar region that presses on spinal nerves can produce symptoms that affect the:
• Low back
• Hips
• Buttocks
• Legs
• Ankles
• Feet
• Toes
Prolapsed Disc Treatment
The type of prolapsed disc treatment prescribed by a physician will depend on the severity and location of the damaged disc. Most patients find that disc prolapse symptoms can be treated conservatively with activity modification, physical therapy, pain and anti-inflammatory medications, stretching, low-impact exercise and/or a limited period of rest. Additionally, some patients find alternative treatments like acupuncture, chiropractic therapy and massage to be highly effective as well.
For pain that is severe or debilitating, a physician might recommend a series of corticosteroid injections, which can reduce painful inflammation to produce relief that lasts for weeks or months. Surgery, while viable for some patients, is usually considered to be a last resort for treating a prolapsed disc, and surgical intervention is typically advised only after several weeks or months of conservative therapy prove to be ineffective for helping you to find symptom relief and achieve a better quality of life.