What is A Slipped Disc?
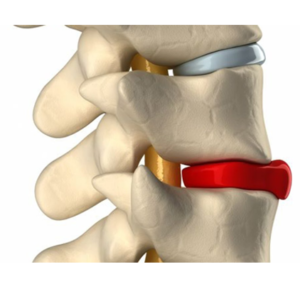
“Slipped disc” is a nonmedical and potentially misleading term used to describe a common degenerative spine condition. The term is deceptive because disc slippage is usually not involved; instead, in some cases, the firm outer shell of a spinal disc is forced outside of its normal boundary. In other cases, a disc will be said to “slip” if it develops a tear in its thick, multilayered wall. This tear can begin from the inside of the disc and work its way outward, or a disc can break open on the outside due to an injury or weak spot.
If a disc tear happens, some of the disc’s gel-like inner core material (nucleus pulposus) can potentially escape the confines of the disc wall and seep into the spinal canal. Also known as a herniated, ruptured or bulging disc, slipped discs can occur in the cervical (upper), thoracic (middle) and lumbar (lower) regions of the spine.
Symptoms of a Slipped Disc
A slipped disc does not always cause symptoms. In general, discomfort arises only if displaced soft tissue irritates the damaged disc wall or compresses a sensitive spinal nerve root or the spinal cord itself. The nature and location of the symptoms will depend on the site of the damaged disc. For instance, a slipped disc in the lumbar spine can cause pain, tingling, numbness, muscle weakness and spasms that radiate from the lower back through the buttocks, hips, legs, and feet. In other cases, a damaged disc in the cervical spine can lead to slipped disc symptoms in the neck, shoulders, arms, and hands. Slipped discs and other degenerative spinal conditions often affect the lumbar region of the spine, which supports much of the body’s weight and therefore is especially prone to damage from the effects of ongoing wear and tear.
Some alternative terms for the condition — such as bulging discs, herniated discs, ruptured discs, and torn discs — are far more descriptive of what actually occurs within the spine when a disc is damaged.
Causes of a Slipped Disc
In most cases, a slipped disc results from the cumulative effects of ongoing wear and tear on the spinal anatomy. As part of the natural aging process, the discs gradually lose water content and elasticity. This is problematic because, in order to function properly, the discs must be supple and pliable.
A well-hydrated and flexible disc can effectively cushion the adjacent spinal vertebrae and support a wide range of motion. Conversely, a dry and brittle disc will lose height and elasticity, making it more susceptible to further damage from the continual stress of daily activities. Even mild pressure on a compromised disc can force its outer wall past its normal boundary, which is a bulging disc. Stress can also lead to the formation of small tears that gradually worsen and herniate, or form a rupture that results in a ruptured or herniated disc.
Sometimes injuries resulting from a forceful, direct blow to the spine can lead to the sudden onset of a slipped disc. Also, people who experience traumatic spine injuries as children or teenagers tend to be more likely to develop disc problems later in life.
Risk Factors for a Slipped Disc
While aging is unavoidable, certain lifestyle factors — such as having poor posture, regularly lifting heavy objects, participating in high-impact sporting activities, smoking and carrying excess body weight — can accelerate the spinal degeneration process. Workers in occupations that require repetitive lifting, bending and twisting, as well as those in jobs that involve whole-body vibration, such as long-distance truck driving, and long periods of sitting, also have a heightened risk of developing degenerative spine conditions. In general, the level of risk increases along with the length of time an individual performs such work.
Additionally, some individuals are genetically predisposed to developing degenerative spine conditions such as a slipped disc.
Slipped Disc Treatments
If you’ve been diagnosed with a slipped disc, your doctor will likely prescribe conservative treatments such as rest, pain medication or lifestyle changes to begin with. These nonsurgical treatments can be highly effective at controlling pain and discomfort and can help many patients avoid the need for a slipped disc surgery. In most cases, doctors will recommend a combination of conservative options for the first few weeks of treatment, using a process of trial and error to identify a plan that works for each individual patient. The most common conservative treatment options include:
- Over-the-counter pain relievers such as acetaminophen. These drugs either increase the body’s pain threshold, so that a person must experience more pain than usual for the body to register the sensation, or block the enzymes that produce pain-sensing chemicals in the body.
- Anti-inflammatory medications, including over-the-counter options or prescription steroids. Both options can help reduce swelling, in turn relieving pressure on an irritated nerve or compressed nerve root. While over-the-counter options like ibuprofen can be taken for a longer period of time, oral steroids are usually only prescribed for a one- or two-week cycle.
- Physical therapy and exercise. An experienced physical therapist can create an individualized plan of stretches and exercises to help you minimize the symptoms of a slipped disc. For instance, a physical therapist may recommend core strengthening and stability exercises along with stretches to increase flexibility and range of motion.
- Lifestyle changes. While the activities recommended by a physical therapist can be helpful, certain everyday activities may make the pain of a slipped disc worse. For example, lifting heavy objects, bending or twisting, participating in high-impact sports or sitting for prolonged periods can all exacerbate neck and back pain. Limiting or avoiding these activities can help minimize discomfort.
- Heat therapy or cold therapy. Many patients find applying heat or ice to the area where the slipped disc is located can lead to short-term relief. This can be repeated as needed.
- Epidural steroid injections. This treatment is often suggested after other conservative therapies but before surgery. During an epidural steroid injection, a longer-lasting corticosteroid and a shorter-term numbing agent are injected directly into the epidural space of the spine. One injection may provide adequate relief for slipped disc symptoms, or patients may receive a series of injections over a period of a few weeks or months. However, physicians typically limit the number of injections a patient can receive over the course of a year, as repeated injections can cause complications.
Your doctor might also recommend certain lifestyle changes when he or she diagnoses you with a slipped disc. For instance, most patients are advised to maintain a healthy weight, as carrying excess weight can increase the amount of strain placed on the spine. Exercising regularly — either to assist with weight loss or improve general fitness — is also recommended, although you should choose activities that do not cause vibration or heavy impact on the spine. Additionally, patients who smoke or drink alcohol are often advised to quit.
Slipped Disc Surgical Treatments
Most people start to experience improved symptoms after just a few months of slipped disc treatment. However, if you continue to experience severe, limiting pain that persists after nonsurgical treatment, slipped disc surgery may be advised. Laser Spine Institute provides outpatient, minimally invasive spine surgery that addresses the symptoms of a slipped disc without the need for traditional open back surgery.