What is Spondylosis?
Spondylosis is a general medical term that is used to describe various forms of spinal degeneration that accompany the natural aging process. Physicians may use the term more specifically to describe the presence of spinal osteoarthritis or degenerative disc disease. If you have been diagnosed with spondylosis, you should ask your doctor about your specific type of spondylosis so you can begin understanding what may have caused your condition and the treatment options available to you.
Causes & Risk Factors of Spondylosis
In most cases, spondylosis is caused by the cumulative effects of ongoing wear and tear on the spine. Spondylosis occurs when the soft tissues in the spinal anatomy — the spinal discs, tendons, muscles, ligaments, and cartilage that lines the facet joints — naturally deteriorate over time. For instance, the spinal discs, which are normally saturated with water, can become dehydrated and lose their effectiveness as cushions between the vertebrae. The cartilage in the facet joints can gradually wear away, resulting in bone-on-bone contact between the joints. This friction can cause inflammation and trigger the body’s natural protective responses, including the production of smooth bony deposits (called bone spurs or osteophytes) in the affected areas. Additionally, the muscles that support the spine can weaken, while ligaments and tendons can thicken, tighten and stiffen.
Spondylosis is also used to refer specifically to spinal osteoarthritis, which is a common result of the natural aging process. Osteoarthritis is an age-related condition that is characterized by the deterioration of the cartilage that covers the joints in the body, including the spine’s facet joints. These joints, which are located between the individual vertebrae, serve an important function in providing the spine with an essential range of motion, allowing it to bend, twist and flex. The cartilage, a smooth, rubbery tissue that covers the ends of the bones in the joints, reduces friction and helps the bones to glide smoothly over each other. When the cartilage breaks down, painful joint damage can occur.
Some people experience more degenerative changes related to spondylosis than others, but most have at least some signs of spinal deterioration that are readily apparent in an X-ray, MRI or CT scan by the age of 40. These findings might include bulging or herniated discs, as well as bone spur formations in the vertebrae affected by degeneration.
There are a number of risk factors that can increase your likelihood to develop spondylosis which include:
- Obesity
- Genetic predisposition
- History of traumatic injuries
- Participation in high-impact sports
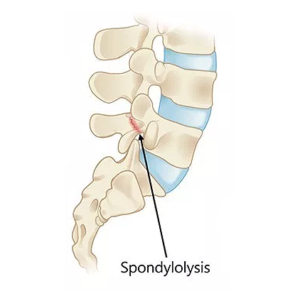
Types of Spondylosis
Spondylosis is classified by its regional location on the spine. The spine consists of 33 vertebrae, 24 of which are individually stacked to create the cervical (upper), thoracic (middle) and lumbar (lower) regions, while nine fused vertebrae make up the sacrum and coccyx (tailbone).
- Cervical spondylosis: Affects the seven cervical vertebrae (C1-C7) that make up the neck region; deterioration is common in this area, mainly because these vertebrae are highly mobile and support the weight of the head
- Thoracic spondylosis: Affects the 12 thoracic vertebrae (T1-T12); deterioration in the middle back is relatively uncommon because the spine in this area is connected to and supported by the ribcage
- Lumbar spondylosis: Affects the five lumbar vertebrae (L1-L5); degeneration is prevalent in this area of the spine because the vertebrae in the lower back support the majority of the body’s weight and facilitate a wide range of motion
- Multilevel spondylosis: Affects the spinal components in more than one region
Common Spondylosis Symptoms
Spondylosis symptoms can range in severity depending on the damage, location, and presence of other spinal conditions. You may have spondylosis and not experience any symptoms. In fact, this condition can go undetected unless the facet joints become painfully stiff, or the spinal cord or nerve root is irritated or compressed by a bone spur or displaced disc material.
The most common general spondylosis symptoms include:
- Localized pain in the affected area of the neck or back
- Numbness or loss of sensation
- Muscle weakness
- Traveling pain, numbness, and tingling
Spondylosis symptoms due to spinal osteoarthritis include:
- Facet joint warmth and stiffness
- Localized aching in the neck or back
- Reduced range of motion in the spine
These symptoms are often worse in the morning or after you wake up, but it’s common for them to improve slightly as you get out of bed and start to move about. Some patients have difficulties standing up or develop a “hunched” posture.
Non-Surgical Treatment for spondylosis
Many patients are able to find sufficient relief from their spondylosis symptoms by using one or more conservative (nonsurgical) treatments. Rather than addressing the underlying cause of the symptoms, conservative treatments are designed to manage discomfort.
Nonsurgical treatment options for spondylosis
- Over-the-counter pain relievers — such as acetaminophen, which can relieve pain (but do not address inflammation)
- Nonsteroidal anti-inflammatory drugs (NSAIDs) — such as ibuprofen and naproxen, which can reduce inflammation that is causing pain
- Prescription pain relievers — which can address severe pain that does not respond to over-the-counter medications
- Facet joint injections — which numb pain in arthritic joints and can also help physicians to locate which joints are causing the worst pain
- Epidural steroid injections — which can reduce severe inflammation around a compressed nerve root while temporarily numbing the area
Most likely, your spondylosis symptoms are causing you discomfort and you probably would prefer to rest, engaging in physical activity and exercising might seem a bit counterintuitive. However, a physical therapist can recommend a course of targeted stretches and exercises, which can be very beneficial in enhancing the strength and flexibility of the spine and its supporting muscles. This, in turn, can facilitate a greater range of motion and healing. You may also find relief through alternative treatments like yoga and acupuncture. Of course, one or two days of taking it easy is generally acceptable if pain prohibits any regular activity, but you should keep in mind that remaining inactive for too long can actually be harmful, possibly resulting in decreased circulation, joint stiffening, and blood clots.
Surgical Treatment for Spondylosis
If spondylosis symptoms are debilitating or persist after several weeks or months of conservative treatment, surgery may be recommended. However, patients who are considering surgical intervention should be aware that a highly invasive open spine procedure is not the only avenue to relief. Some patients are candidates for the advanced minimally invasive spine surgery performed by the surgeons at Laser Spine Institute. Our skilled surgeons perform these procedures on an outpatient basis, so most of our patients are able to go home within hours of their surgery.